Pain
Diagnosing Degenerative Disc Disease (DDD)

What is degenerative disc disease?
Degenerative disc disease (DDD) is a condition of the spine, in which one or more of the discs between the vertebrae, also known as intervertebral discs, cause neck or back pain. Intervertebral discs are the cushions between the vertebrae; they keep the back pliable and enable the body to bend, twist, and carry weight. Intervertebral discs are mainly composed of water, and as a person ages, the discs dry out, lose their flexibility, elasticity, and the ability to absorb shock. When this causes pain, it is referred to as degenerative disc disease.
Diagnosing degenerative disc disease
Degenerative disc disease can be a difficult condition to diagnose as it progresses slowly and can involve multiple complications, so it may initially present as another medical condition.
Primary care doctor visit
The first step in the diagnostic process involves a visit to a primary care doctor. Obtaining a medical history is typically the first tool used in the diagnostic process. Questions regarding pain onset, severity, duration, and location; family history of back problems; recent accidents or injuries; and current treatment methods are typically asked.
A physical examination typically follows the medical history. The physician feels the spine to see if any abnormalities or areas of increased pain are present. The individual is usually asked to do certain movements, including walking, to determine their range of motion. The doctor may also check reflexes to determine if nerve damage is involved.
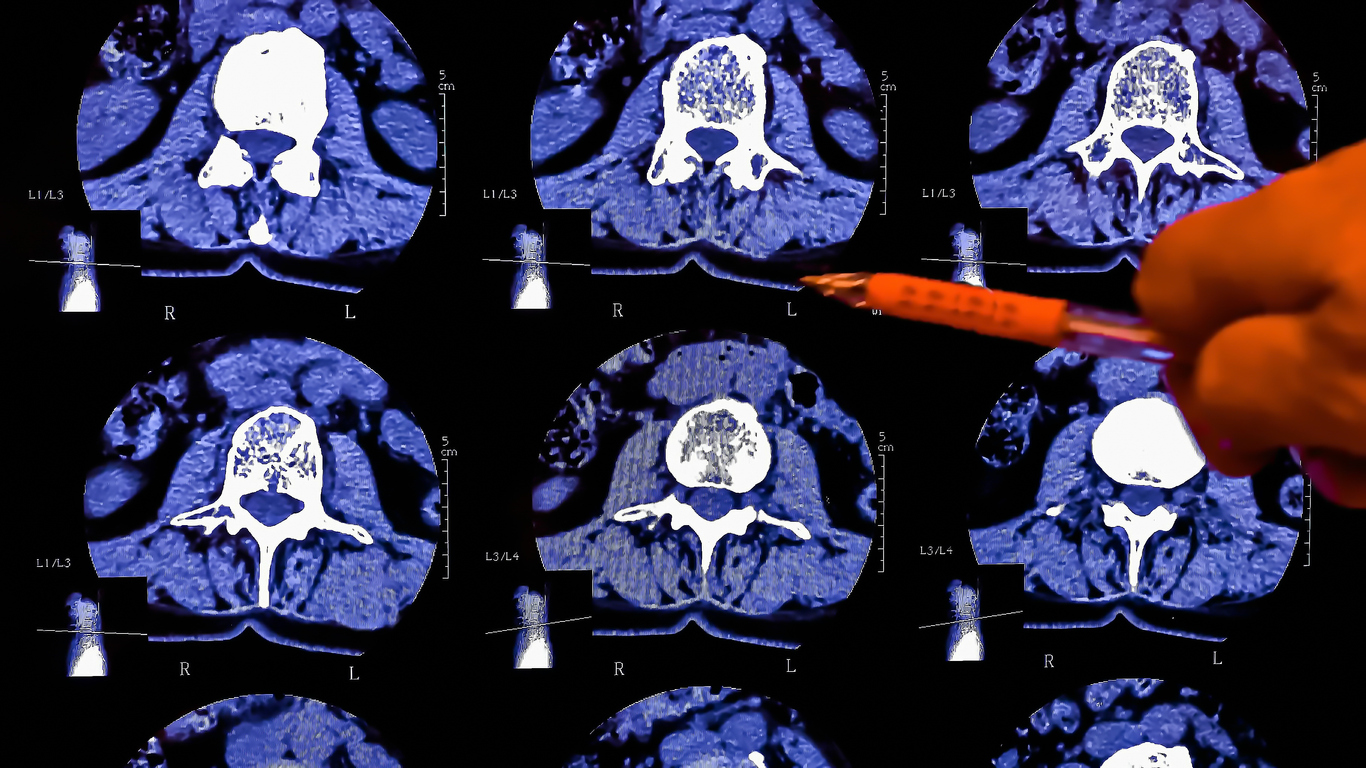
After the physical exam, the primary care doctor may order diagnostic tests, such as blood work, X-rays, CT scans, or MRI imaging. Based on the test results, medical history, and physical exam, the primary care doctor may have enough information to confirm or eliminate a diagnosis of degenerative disc disease; if not, the doctor may make a referral to a spine specialist.
Specialist visit
During an initial visit to a spine specialist (neurosurgeon, orthopedic surgeon, orthopedist, physiatrist, neurologist, etc.) any information sent by the primary care doctor is reviewed. The specialist will likely obtain a medical history and perform a physical examination. They may also order more blood work, X-rays, CT scans or MRI imaging.
A spine specialist may also order further testing, such as a bone scintigraphy, an electromyography, or a nerve conduction test. Bone scintigraphy is a nuclear medicine test that involves injecting a dye with a radioactive marker that shows where the dye is being absorbed into the bone. Areas that absorb more dye (“hot spots”) indicate abnormal activity, such as inflammation. A bone scintigraphy provides very detailed images of possible damage to the spine. If concern is present regarding possible nerve involvement or nerve damage, an electromyography (EMG) or a nerve conduction test may be ordered.
Diagnostic procedures
Two procedures may be used to diagnose degenerative disc disease: a discogram (discography) and a myelography. These procedures are done either by a spine specialist or a neuroradiologist.
A discogram, or discography, is a procedure that identifies the specific discs that are causing pain. Before the procedure, a medication is given intravenously for relaxation purposes. A health care provider cleans the skin and uses a local anesthetic to numb the area. Once numb, the provider inserts a small needle — with x-ray guidance — into the center of a spinal disc. This is then repeated for all discs in question. Once all the needles are in place, the health care provider injects a small amount of contrast dye into the disc(s). If a disc is a source of pain, the injection causes temporary pain and other related symptoms. If a disc is not affected by degenerative disc disease, no discomfort is felt from the injection.
A myelography is an imaging procedure used to evaluate the spinal cord. The image it produces is known as a myelogram. This procedure is helpful in diagnosing disorders of the spine that cause myelopathy or spinal compression. Myelography involves the injection of contrast dye and the use of X-ray, CT or MRI scans to obtain images of the spine. To begin, the skin is cleaned and local anesthetic is used to numb the area. Once the area is numb, a contrast dye is injected into the space around the spinal cord. After waiting a few minutes for the contrast dye to work, imaging tests are performed. Some pain or pressure may be felt when the contrast dye is injected.
After diagnosis
Once a diagnosis of degenerative disc disease is confirmed, treatment options will be discussed. Depending on the severity of the condition, treatment options include at-home management, conventional medical treatment options, alternative and complementary treatment options, or surgery.