Pain
Diagnosing Failed Back Surgery Syndrome
What is failed back surgery syndrome?
Failed back surgery syndrome (FBSS) occurs when a spine surgery does not relieve the back pain that was present before the surgery. FBSS does not necessarily mean a problem occurred during the surgery; however, it does mean that one of the intended outcomes of the surgery — the reduction or elimination of pain — has failed.
FBSS occur weeks, months or years after back surgery. Most physicians will diagnose FBSS if pain persists six to 12 months after a successful surgery. Obtaining a correct diagnosis can help determine treatment options.
Diagnosing failed back surgery syndrome
The diagnostic process typically begins with a detailed medical history, emotional well-being exam, and questions about lifestyle choices. A physician then reviews the individual’s symptoms, conducts physical and neurological exams, and orders imaging tests to aid in diagnosis.
Review of medical history
A medical history should include information about any allergies, previous and current diagnoses, medical conditions, vitamin and supplement use, and over-the-counter and prescription medications. A health care provider should also be made aware of any previous or current treatments (e.g., physical therapy, injections, chiropractic, etc.) and their effectiveness.
Assessment of emotional well-being and lifestyle choices
Mental and emotional health issues, such as depression and anxiety, should be disclosed during the diagnostic process. Lifestyle information, such as diet, smoking, sleep issues, and exercise habits, can help determine factors that contribute to FBSS.
Assessment of symptoms
Symptoms should be discussed in as much detail as possible. Typically, questions about pain levels, location, time of onset, level of consistency, etc., are asked. Any bowel or bladder issues or nerve symptoms should also be disclosed.
Physical exam
A physical exam typically includes a physician palpating parts of the spine and back to determine areas of tenderness, inflammation or spasms. Certain movements, such as walking, bending, standing or twisting, are assessed to check gait, balance and posture issues. Diagnostic tests, such as the straight leg raise test, can help identify the specific location of pain.
Neurological exam
A neurological exam can help identify muscle weakness, abnormal sensations, nerve health, nerve dysfunction, and radiculopathy. A cotton swab or pin is moved across the skin to test sensation in the extremities. Arms and legs are checked for weakness and reflex issues.
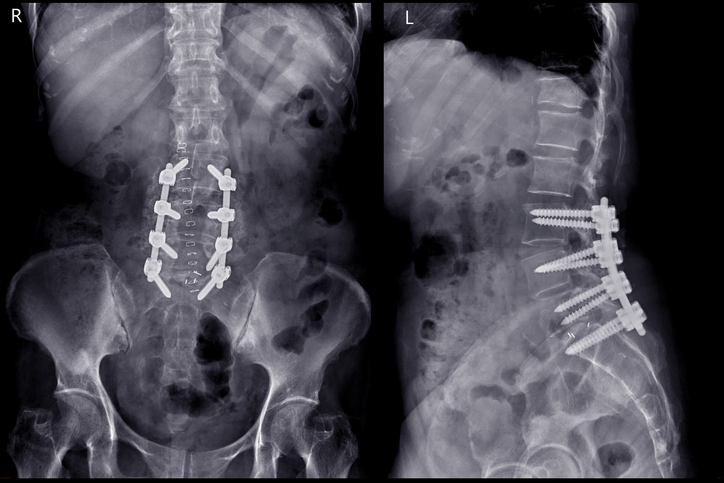
Imaging tests
Imaging tests, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI), provide valuable information and help confirm a diagnosis. CT or MRI scans, with and without contrast, can show areas of concern.