Pain
Failed Back Surgery: New Hope for Those Living in Pain

What is failed back surgery syndrome?
Failed back surgery syndrome (FBSS) occurs when a spine surgery does not relieve the back pain that was present before the surgery. FBSS does not necessarily mean a problem occurred during the surgery; however, it does mean that one of the intended outcomes of the surgery — the reduction or elimination of pain — has failed.
An FBSS diagnosis requires that back pain is linked to spinal surgery. In order to be diagnosed with FBSS, the pain must continue, reoccur, or worsen after the expected healing time has elapsed, however, not after too much time has passed following surgery that it could be caused by another health issue. For example, if an individual undergoes surgery for a herniated disc, then two years later develops back pain because the herniation recurs, they may be diagnosed with FBSS. If someone develops back pain 12 years after back surgery, it is highly unlikely that they will be diagnosed with FBSS.
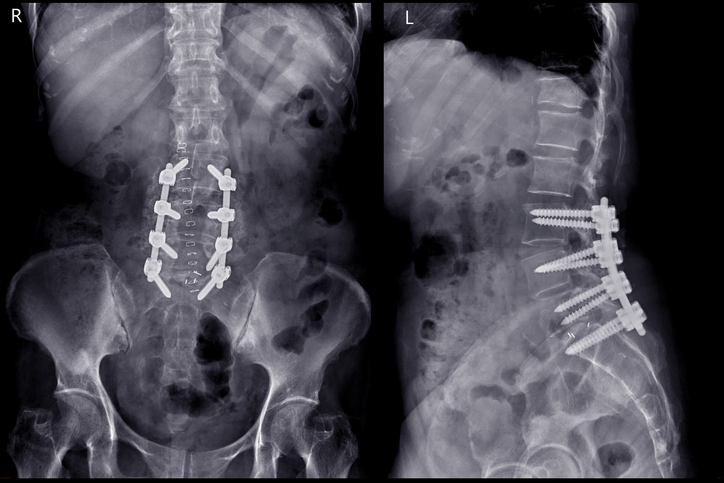
FBSS treatment
An interdisciplinary approach is often recommended for FBSS. This includes, but is not limited to, the following:
- Medication
A wide variety of medications are available to treat back pain. They include non-steroidal anti-inflammatory drugs (NSAIDs), such as naproxen and ibuprofen, opioid pain medications, muscle relaxers, anticonvulsants, or antidepressants. - Epidural injections
Epidural injections consist of delivery of medicine into the epidural space via a syringe. The epidural space is the fat-filled area covering the spinal cord. It protects the spinal cord and surrounding nerves from damage. Many people confuse an epidural anesthesia injection, widely known to relieve pain as women are giving birth, with an epidural steroid injection. - Sacroiliac (SI) joint injection
The sacrum at the bottom of the spine connects to each side of the pelvis by the sacroiliac joints. These joints absorb shock and tension between the upper and lower body. Too little or too much motion of one or both joints can cause pain due to inflammation. An SI joint injection may be used to soothe sacroiliac joint pain through a combination of anesthetic and anti-inflammatory medications that reduce inflammation in the joint and the surrounding nerve tissue. Breaking the pain cycle makes it easier for the body to heal itself naturally. - Radiofrequency ablation
Radiofrequency (RF) ablation treatment is a drug-free therapy that involves the movement of energy to destroy abnormal tissue that may cause pain or disease. RF ablation is a minimally invasive procedure that uses an electrical current to burn nerve tissue and reduce pain signals. This treatment is commonly used in the management of spinal and neuropathic (nerve damage) conditions. - Facet joint injection
Facet joints are small joints located between each vertebra of the spine. A pair of facet joints are located at the back of each spinal segment. These joints help support the spine and allow for range of motion. During facet joint injections, a small amount of local anesthetic and steroid medication is injected into one or more facet joints. A local anesthetic provides immediate pain relief, while a steroid medication reduces inflammation and provides long-lasting pain relief. - Spinal cord stimulator
A spinal cord stimulator (SCS) is a small, implanted device that uses tiny electrical impulses to mask pain signals from reaching the brain. Spinal cord stimulation therapy is an opioid-free, medication-free, FDA approved treatment for chronic pain.