Pain
Diagnosing Lyme Disease

What is Lyme disease?
Lyme disease, or Lyme borreliosis, is an infectious disease caused by the bacteria Borrelia. The bacteria Borrelia burgdorferi and Borrelia mayonii are responsible for Lyme disease in North America. In Europe and Asia, Borrelia afzelii and Borrelia garinii are responsible for Lyme disease. The bacteria is spread to humans via the bite of an infected tick, usually a black-legged tick (commonly known as a deer tick).
Diagnostic difficulties
Lyme disease is often difficult to diagnose. Many of the common symptoms, such as headache, fatigue, and joint pain, mimic symptoms of a variety of other health conditions. The “bull’s-eye” rash (erythema migrans), the most distinctive symptom, does not appear in every case of Lyme disease; in fact, approximately 25% of individuals with Lyme disease do not experience a rash. Diagnostic tests that are currently available have limitations; they cannot diagnose early Lyme disease as it takes time for the body to produce antibodies that the tests measure.
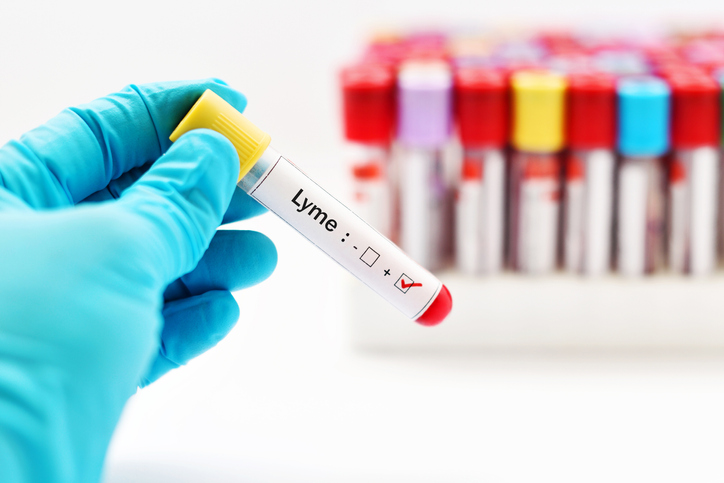
Tests for Lyme disease
Two tests are commonly used to diagnose Lyme disease: an ELISA test and a Western blot test.
ELISA test
An ELISA test is a blood test that detects antibodies that the body produces in response to the bacterium B. burgdorferi. If done too early or too late, it can give a false negative result.
Western blot test
A Western blot test also detects antibodies that the body produces in response to the bacterium B. bugdorferi. This test detects two different classes of antibodies: IgM and IgG. IgM antibodies develop faster, within the first 4 weeks of infection, but are more likely to give a false positive. Testing for IgG antibodies is more reliable, but IgG antibodies take up to 4-6 weeks to develop to a measurable level. Up to 20% of Lyme disease cases are missed by this test.
If Lyme disease is suspected, the CDC recommends that an ELISA test is done first. If the ELISA test comes back positive or is uncertain, then a Western blot test should be done. It should be noted that not all organizations agree with the testing protocol to eliminate the possibility of Lyme disease, including the International Lyme and Associated Diseases Society (ILADS).
Important factors in making a Lyme diagnosis
The following factors should be considered during the diagnostic process:
- Tick bite and exposure risk
Even if an individual does not remember being bitten by a tick, a Lyme disease diagnosis is still possible. Recent exposure risks, such as activities (i.e. hiking, camping), location, and any travels are taken into consideration. - Rash/Erythema migrans
A “bull’s-eye” rash is a classic indicator of Lyme disease, but the rash does not always appear as a “bull’s-eye,” and a rash does not appear in every case of the disease. It is important to note that other tick-borne infections can also cause rashes. - Other possible conditions
Lyme disease symptoms can mimic those of various health conditions, including rheumatic and neurological conditions. Unfortunately, undiagnosed, long-lasting cases of Lyme disease can be misdiagnosed as somatoform disorders. - Testing
If an erythema migrans rash is present and symptoms match those of Lyme disease, testing is generally not necessary. Testing is often used in other cases with the caveat that testing too soon or too late can result in a false negative. A negative test result alone should not be the only reason for ruling out a Lyme diagnosis.
Diagnosing Lyme disease is not a simple process. It requires identifying possible tick exposure, assessing physical symptoms, and laboratory testing. A diagnosis is best made when considering each of these factors.
If Lyme disease is suspected, seeking a health care professional who is experienced with diagnosing and treating Lyme disease is essential. The International Lyme and Associated Diseases Society (ILADS) provides a list of Lyme-aware doctors.