Pain
Diagnosing Peripheral Neuropathy

What is peripheral neuropathy?
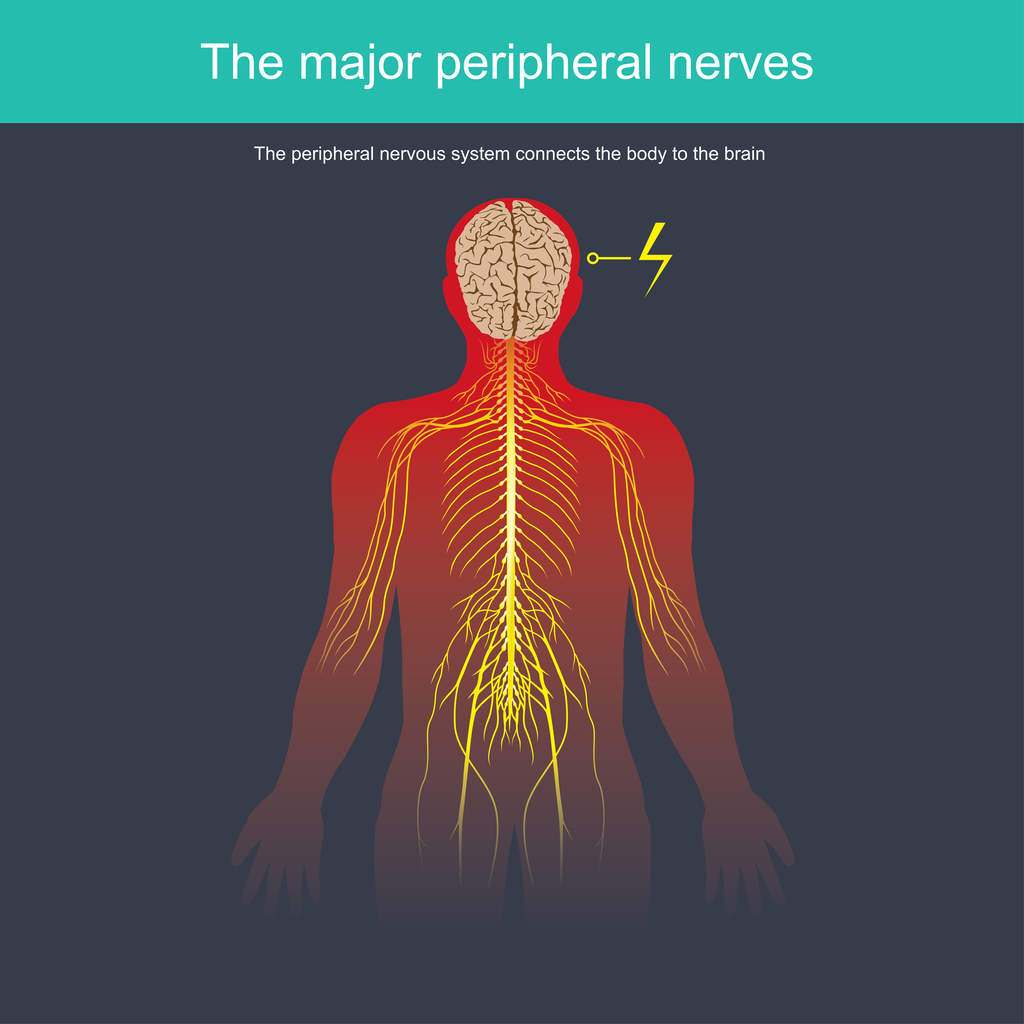
Peripheral neuropathy develops as a result of nerve damage to the peripheral nervous system. The peripheral nervous system is the communication network that connects the central nervous system (the brain and spinal cord) to the rest of the body (muscle, skin, internal organs, etc.). Approximately 20 million people in the United States have some type of peripheral neuropathy.
What are the symptoms of peripheral neuropathy?
Symptoms of peripheral neuropathy depend on the type of nerves that are damaged. Nerves are categorized into motor, sensory, and autonomic. Motor nerves control the movement of muscle; therefore, motor nerve damage will often cause muscle weakness. The function of sensory nerves is to receive sensation. If sensory nerves are damaged, temperature, pain, vibration or touch can be impaired. The autonomic nerves regulate heart rate, blood pressure, bladder function, and digestion. Autonomic nerve damage can cause heat intolerance, altered sweating, loss of bladder control, dizziness, lightheadedness, intestinal muscle contractions, or difficulty eating/swallowing.
How is peripheral neuropathy diagnosed?
Diagnosing peripheral neuropathy can be challenging due to the numerous causes and varying symptoms. The diagnostic process includes a medical history, physical and neurological examinations, blood and urine tests, nerve function tests, imaging tests, or nerve/skin biopsies.
Medical history
The diagnostic process begins with a health care professional asking questions about the individual’s medical history (symptoms, symptom triggers, symptom relief factors, current medication regimen, social and work habits, alcohol use, infectious disease exposure, family health history, and exposure to toxins).
Physical and neurological examination
A health care provider will check reflexes, muscle tone and strength, posture, and coordination.
Blood and urine tests
Blood and urine tests may be ordered to identify any vitamin deficiencies, metabolic disorders, infections, diabetes, genetic defects, thyroid conditions, abnormal immune function, or underlying diseases that may be causing neuropathy symptoms.
Nerve function tests
- Electromyography (EMG)
An electromyography involves the insertion of very thin needles into specific muscles to determine nerve and muscle function. An EMG helps identify motor neuropathy and differentiates between nerve and muscle conditions. - Nerve conduction velocity (NCV)
A nerve conduction test involves the placement of electrodes on different areas of the skin. A low electrical current is used to stimulate the nerve fibers to determine how strongly and quickly the nerves transmit signals. An NCV helps identify whether neuropathy symptoms are caused by degeneration of the myelin sheath or the axon. - QSART test
A QSART test measures the body’s ability to sweat in several locations on the arm(s) and leg(s). This can help identify small fiber polyneuropathies. - Autonomic reflex screen
An autonomic reflex screen identifies how well the autonomic nerve fibers work. - Sensory tests
Various sensory tests can be used to determine how the body responds to touch, temperature and vibration.
Imaging tests
- Computed tomography (CT)
A CT scan of the spine can reveal narrowing of the spinal canal (spinal stenosis), herniated discs, tumors, cysts, and any vascular abnormalities. - Magnetic resonance imaging (MRI)
An MRI of the spine can provide more detail than a CT scan regarding any nerve root compression and other abnormalities.
Nerve or skin biopsies
- Nerve biopsy
A nerve biopsy involves the removal of a small portion of nerve tissue — typically tissue from a sensory nerve in the lower leg (sural nerve biopsy) — to identify the type and cause of neuropathy. - Neurodiagnostic skin biopsy
A neurodiagnostic skin biopsy involves the removal of a tiny piece of skin to identify any reduction in nerve fiber endings.