Pain
Multiple Sclerosis
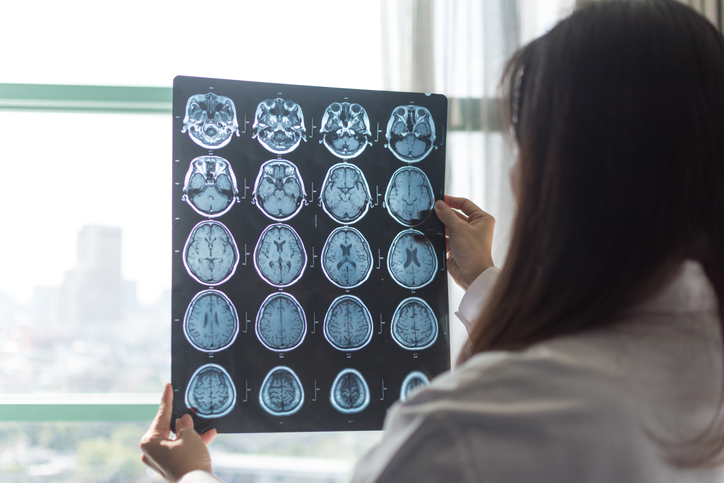
Multiple sclerosis or MS is an immune-based inflammatory disease that affects the myelin, the protective cover of nerve fibers. This causes inflammation, scar tissue and/or lesions in the brain. MS can differ depending on what nerves are affected by demyelination. There are 4 different types of multiple sclerosis.
28 people found this helpful
Print
Share
Save
Did you find this helpful?
You may also like