Pain
The Role of the Gut in Neuropathic Pain

What is neuropathic pain?
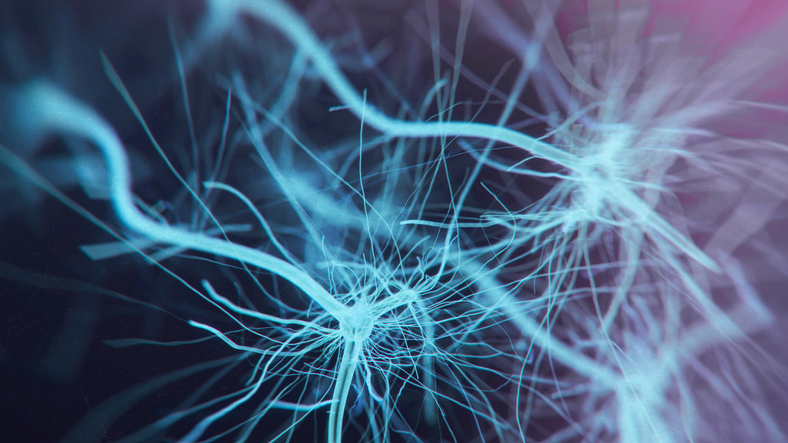
Neuropathic pain occurs when the central nervous system or the peripheral nerves are damaged. Peripheral neuropathy usually begins in the longest nerves of the body, such as the feet and hands. As the condition progresses, it moves up the arms and legs.
Because the spine and nerves are intertwined and work together, issues in the spine can cause nerve pain. Lumbar herniated disc is a common form of nerve pain that occurs when a disc between the vertebrae becomes herniated and places pressure on a spinal nerve root. Once the nerves become damaged and neuropathy becomes an issue, false signals are sent from the peripheral nervous system and central nervous system to the spinal cord, and then to the brain.
The gut and neuropathic pain
A link was discovered over a decade ago between inflammatory bowel disease and certain conditions, including carpal tunnel syndrome, small fiber neuropathy, and sensorimotor polyneuropathy. Research conducted confirmed that the line of communication between the gut and brain has an impact on various systems of the body, including immune, endocrine, metabolic and neural.
The link between gastrointestinal disorders and neuropathic pain is unclear. Most current available treatment plans do not remedy the underlying cause of pain. Investigating the gut microbiome, however, could help determine the cause of neuropathic pain. Numerous neurological and metabolic connections between the gut and the central nervous system have shown to be regulated by the gut microbiome.
In an animal study, chronic constriction injury was shown to cause extreme increased sensitivity and alteration in the gut microbiome. The changes in the gut microbiome were similar to those shown in cognitive impairments, stroke, and sleep deprivation. The injury was also shown to alter the metabolism in the serum and spinal cord. Additional studies are needed on human patients; however, these findings may provide beneficial treatment options for neuropathic pain. This could include a low FODMAP diet, improved emotional approaches to stress management, fecal transplant, probiotics, antibiotics, and vitamin D supplements.