Pain
Diagnosing Psoriasis

What is psoriasis?
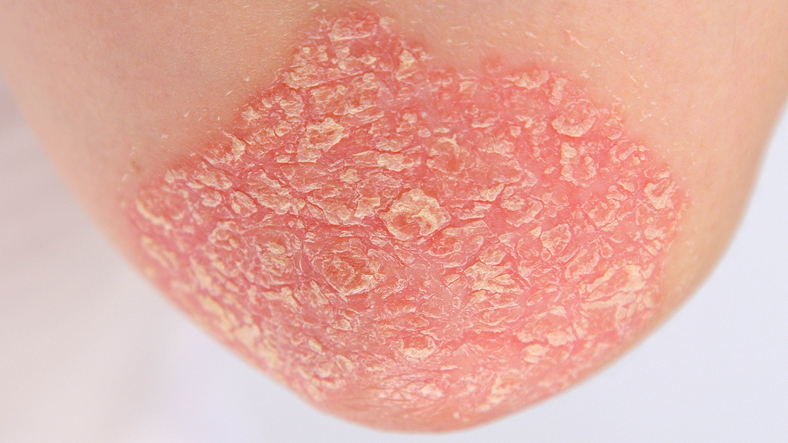
Psoriasis is an autoimmune disease that causes skin cells to multiply up to 10 times faster than normal. There is a wide spectrum of severity and manifestations of psoriasis, but common characteristics of most types of psoriasis include skin redness (erythema), thickening, and scaling (squamae).
Symptoms of psoriasis range from pinhead-sized spots on the skin to major eruptions that cover large areas of skin. Symptoms most commonly occur in cycles, flaring for a few weeks or months, then subsiding or going into remission.
Diagnostic process
The diagnosis of psoriasis is primarily made through clinical examination. However, in some cases, a skin biopsy or other medical tests may aid in the diagnosis.
Clinical examination
A medical history and physical examination are the most common diagnostic tools used for psoriasis. Clinical clues that suggest psoriasis include the following:
- A physical examination of the skin and scalp that reveals erythema (redness), thickening, and squamae (scaling)
- A family history of psoriasis
- Evidence of joint pain, swelling or stiffness
- A recent illness or increased stress
Skin biopsy
A sample of skin may be biopsied for examination under a microscope. A biopsy is usually reserved for atypical presentations of psoriasis or to exclude other disorders, such as eczema or skin infections. Common types of skin biopsies include the following:
- Punch biopsy
A punch biopsy involves the use of a round, circular tool (similar to a paper-hole punch) to remove a small core of skin. - Shave biopsy
A shave biopsy involves the use of a blade to cut off the outermost layer of skin. - Excisional biopsy
An excisional biopsy involves the removal of an entire lesion on the skin and, in some cases, requires a skin graft to repair the area. - Incisional biopsy
An incisional biopsy involves the removal of a section of a large lesion.
A positive skin biopsy for psoriasis may show a large number of activated T cells; the absence of normal cell maturation; or an increased number of basal cells (known as basal cell hyperplasia). Basal cells produce new skin cells.
Other laboratory tests and studies
While additional labs, tests and studies are not usually needed to diagnose psoriasis, any of the following may be ordered:
- Fungal studies
Fungal studies may be ordered to rule out fungal infections. - Erythrocyte sedimentation rate (ESR)
An ESR blood test may be ordered to check for systemic inflammation. ESR may be elevated with pustular or erythrodermic psoriasis. - Autoantibody studies
When psoriatic arthritis is suspected, autoantibody tests may be ordered to rule out other types of arthritis. These tests may include a rheumatoid factor (RF) blood test, which may indicate rheumatoid arthritis; or an antinuclear antibody (ANA) test, which may indicate lupus. - Imaging studies
Images from X-rays and bone scans can aid in the diagnosis of psoriatic arthritis. - Baseline laboratory studies
Baseline laboratory studies may be ordered when starting systemic therapies, such as biologics. Laboratory tests may include a complete blood count (CBC), complete metabolic panel (CMP), hepatitis panel, tuberculosis screening, or pregnancy test.