Pain
What Is Psoriatic Arthritis (PsA)?

Psoriatic arthritis (PsA) is a form of inflammatory arthritis that can occur with the skin condition psoriasis, a condition that causes red, itchy patches and silvery scales on the skin and scalp. PsA is a combination of the joint problems of arthritis and the skin issues of psoriasis. With PsA, the immune system mistakenly attacks healthy cells in the joints and causes overproduction of skin cells. Typically, the skin patches associated with psoriasis appear first, and symptoms of psoriatic arthritis appear later; however, although less common, joint issues can occur before skin patches develop. Approximately 7.5 million Americans have psoriasis, and approximately 30 percent of those people have or will develop PsA.
Types of psoriatic arthritis
Psoriatic arthritis is categorized into five types:
- Symmetric psoriatic arthritis affects the same joints on both sides of the body.
- Asymmetric psoriatic arthritis affects joints on only one side of the body.
- Distal interphalangeal predominant psoriatic arthritis affects the distal joints, which are the joints closest to the nails.
- Spondylitis psoriatic arthritis affects the joints in the spine.
- Psoriatic arthritis mutilans is a severe, deforming type of PsA that typically affects the hands and feet.
What are the symptoms of psoriatic arthritis?
The symptoms of PsA include, but are not limited to, the following:
- Joints that are painful, swollen, and warm to the touch
- Stiff joints
- Swollen fingers and toes
- Foot pain
- Lower back pain
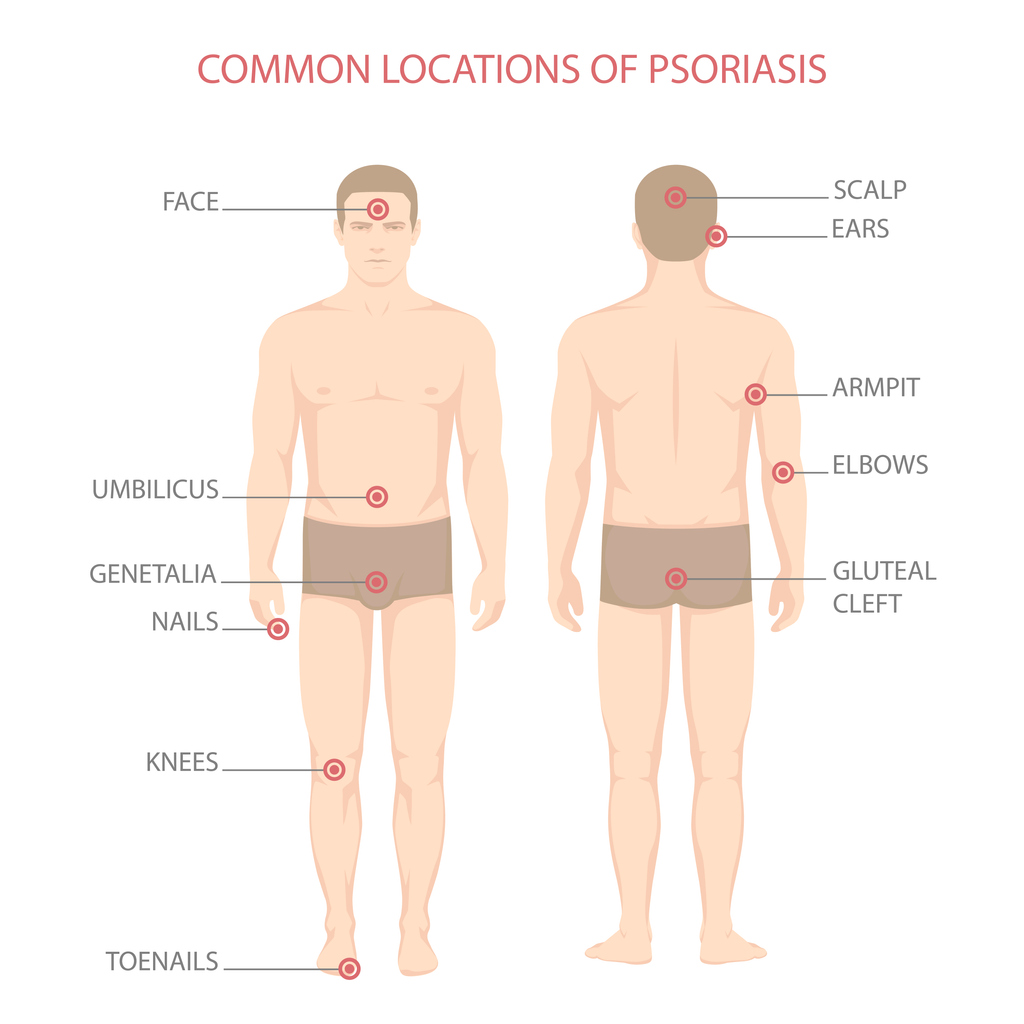
- Scaly skin patches
- Flaky scalp
- Fatigue
- Cracking, pitting, or white spots on the nails
- Separation of the nail from the nail bed
What causes psoriatic arthritis?
Psoriatic arthritis is an autoimmune condition. The immune system mistakenly attacks healthy cells in the joints and causes overproduction of skin cells. Although the exact cause of this immune system reaction is not known, a combination of genetic and environmental factors may play a role. Researchers believe PsA can be triggered by environmental factors, such as infections, extreme stress, or injuries, in those who are genetically susceptible.
Who is at risk for developing psoriatic arthritis?
- Having psoriasis is the biggest risk factor for psoriatic arthritis. Experiencing the psoriasis symptom of pitted, deformed nails especially increases the risk of developing PsA.
- A family history of psoriasis or PsA increases the risk of developing PsA.
- PsA most commonly presents between the ages of 30 and 50.
- Psoriasis and PsA are more common in white people than people of other races.