Pain
Type 1 vs. Type 2 Diabetes
What is diabetes mellitus?
Diabetes mellitus is a metabolic disease that affects the amount of glucose in the blood (blood sugar). The body breaks down food and drinks into a simple sugar called glucose. Glucose is then used by the body as a source of energy for the brain, muscle cells and tissue cells.
Insulin is a natural hormone produced by the pancreas; it transports glucose from the blood to the body’s cells to be stored and used for energy. Diabetes mellitus, or diabetes, occurs when the body doesn’t make enough insulin or can’t effectively use insulin.
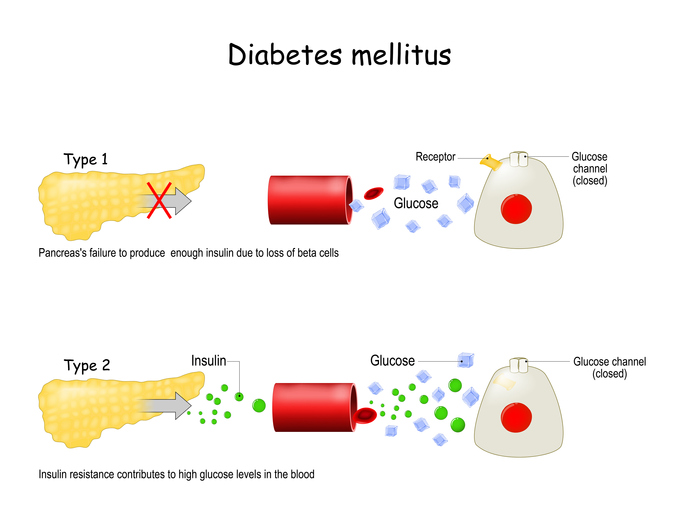
The difference between type 1 and type 2 diabetes
The two main types of diabetes are type 1 and type 2. Both are chronic diseases that affect the way the body regulates blood glucose, or blood sugar. Although both type 1 diabetes and type 2 diabetes can lead to dangerous high blood sugar levels, they differ in a variety of ways.
Type 2 diabetes is the most common type of diabetes. An estimated 90 to 95 percent of individuals with diabetes in the United States have type 2 diabetes.
With type 1 diabetes, the pancreas does not produce enough insulin to regulate glucose; with type 2 diabetes, the body does not respond to the insulin produced, resulting in unregulated blood glucose.
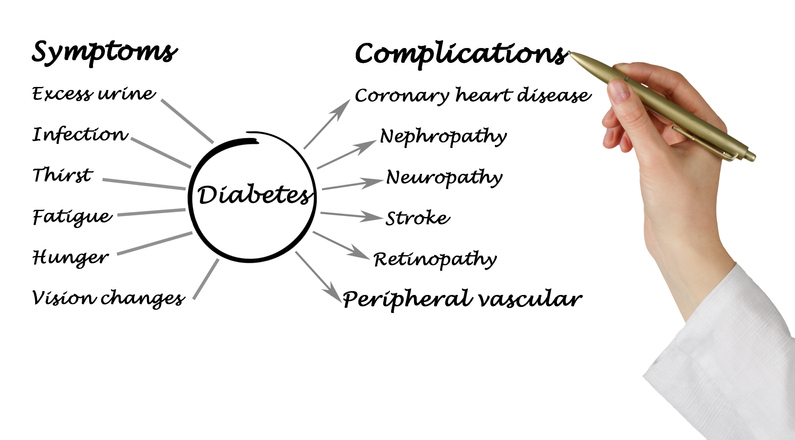
Symptoms
Type 1 diabetes symptoms typically develop quickly; whereas, type 2 diabetes symptoms often don’t appear for many years. Sometimes, symptoms of type 2 diabetes are completely absent, which can result in severe complications due to lack of treatment.
Shared symptoms of type 1 diabetes and type 2 diabetes include the following:
- Frequent urination
- Excessive thirst
- Increased appetite
- Fatigue
- Blurry vision
- Slow-to-heal cuts or sores
Symptoms specific to type 1 diabetes include the following:
- Irritability
- Mood Changes
Causes
Type 1 diabetes is thought to be the result of an autoimmune response that causes the immune system to mistakenly attack and destroy the insulin-producing beta cells in the pancreas. When insufficient or no insulin is made (due to the destroyed beta cells), glucose cannot enter the body’s cells to be used for energy, resulting in high levels of blood sugar.
The exact cause of type 2 diabetes is uncertain; however, both genetic and environmental factors are thought to play a key role. The body produces the proper amount of insulin; however, it cannot effectively use it, resulting in insulin resistance. Prediabetes often leads to type 2 diabetes as cells become resistant to insulin, and the pancreas is not able to produce enough insulin.
Prevention
Type 1 diabetes cannot be prevented. The risk of developing type 2 diabetes can be lowered through lifestyle changes, such as maintaining a healthy weight, increasing activity levels and eating a balanced diet.
Diagnosis
Type 1 diabetes and type 2 diabetes are both diagnosed using a blood test — the glycated hemoglobin (A1C) test. This blood test averages the body’s glucose levels of the previous two to three months. A level of 6.5 or higher is indicative of diabetes.
Treatment
Since type 1 diabetics do not produce insulin, it must be regularly injected into the body. This can be accomplished with injections into the soft tissue or with the use of an insulin pump. Due to frequent fluctuation of blood glucose levels, blood sugar testing is essential in managing type 1 diabetes.
Type 2 diabetes can often be controlled, or even reversed, with diet and exercise. Oral medication(s) or insulin injections may be needed to control blood glucose levels. Health care professionals recommend testing blood sugar levels on a regular basis.